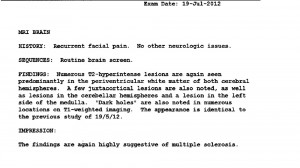
After
meeting Lori Batchelor
last month and thinking about the logic of having good blood flow for a healthy brain, I decided to go to
AIM Medical Imaging
to see whether or not I had narrowed veins. I had heard that Dr. Raj Attariwala was the best diagnostician in Canada, so I booked an appointment for September 30.
The
McMaster Study
showed only one person with MS who had CCSVI out of a hundred. I was eager to challenge that finding as I suspect that many people who do not have MS also have CCSVI. And if it’s only 1/100 for people with MS, then chances were slim that I would have it. It was interesting to note that they were looking specifically for vein blockages, not reduced flow or backwards flow/reflux.
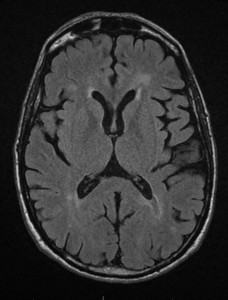
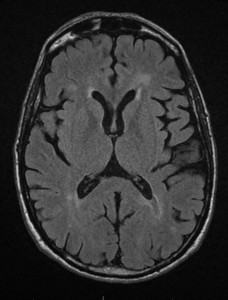
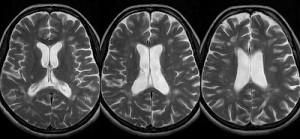
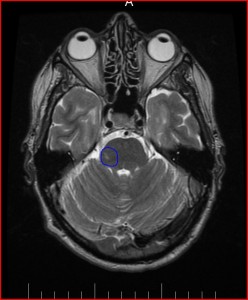
Immediately after the scan, I had a consultation with the radiologist, Dr. Attariwala. I had given him copies of my previous MRIs to look at. Fortunately, there were no new lesions or active lesions.
He was able to identify the lesion in my pons from the very first MRI in May of 2012.
(I wish I had paid for this MRI two years ago as it would have helped guide me better than all the specialists I saw and tests I had. It would have been faster and cheaper and I probably would not have ended up hospitalized twice.)
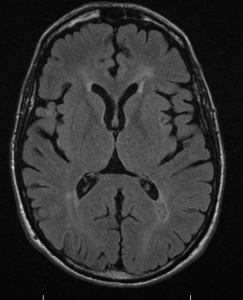
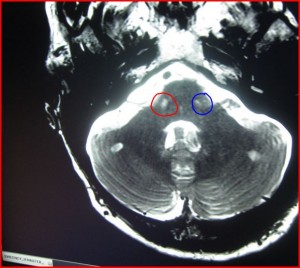
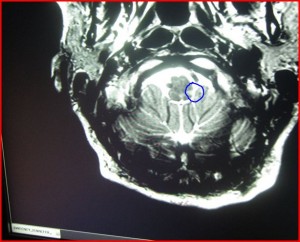
Within a couple of hours, I had images and results. My right jugular vein flows significantly less than my left. This is the opposite of the findings at McMaster where everybody had greater flow in the right than the left. He says that this is a finding that has been “known for years.” (from
extended interview with Dr. Rodger
)

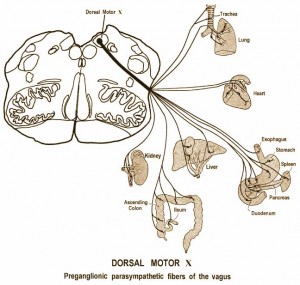
The central vein is called the ‘azygos’ — it was described to me as ‘awful’.
So, it appears to me that I do have CCSVI or chronic cerebrovascular insufficiency according to these images and flow measurements. However, I am not knowledgeable enough to know or assess if I meet the full criteria for CCSVI. This is how it was described in the report:
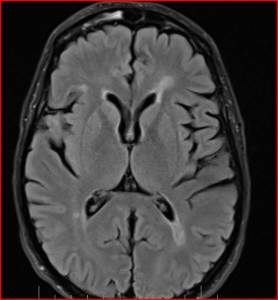
INDICATION: History MS, query jugular venous narrowing.
TECHNICAL Conventional study: axial flair, T2, 3-D space flair, post gad T1sagittal T1 , PD, axial T2 C-spine.
Research: SWI, Venc, azygous, with subtracted multi-sequential venogram through the neck and lower head,
FINDINGS: The patient recognizes that jugular MRI venogram as well as iron deposition sequences remain in the realm of research . . . Known MS demyelination, without MRI evidence of active lesions. To be determined by ongoing research; there is associated substantia nigra iron deposition which is of uncertain significance. The jugular veins demonstrate asymmetry of flow, with the right being diminutive, with transient halting of flow, without reversal. These findings plus the controversial nature of the research component of the study was discussed with the patient.
In the images, I received a graphic representation of the flow measurements taken.
The red line represents flow in the right, the green line in the left. If the red line were to go above the horizontal line at 0, it would indicate backflow or reflux. So, the next step is to investigate further.
There are so many unanswered questions about the procedure and I’m not convinced that some of the research currently being conducted is going to lead to good answers. Most of the research has been looking for gross measures of correlation between blood flow and ways to measure it and assess it, then make pronouncements about the lack of connection with MS, end of story!! For people with MS who have benefited and thrived after the procedure, it has clouded the debate. So many people are looking for a way to end this area of research, calling it a social media phenomenon of unsubstantiated anecdotes. But they are choosing to ignore evidence right in front of them.
I think we need to ask better questions. What’s happening when people get good results from venoplasty? Why aren’t we studying them? Why is there no single-case research being done on an amazing case like Lori Batchelor? Her neurologist is on camera saying that there is improvement when she was diagnosed with secondary progressive MS. How does that happen?