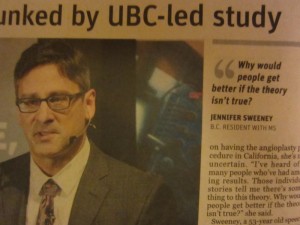
Dr. Anthony Traboulsee
Last week, I attended a radiology grand rounds session at VGH on CCSVI in MS, titled “Observations on extracranial venous anatomy in MS: An update on CCSVI research.”
I wanted to understand the study without the media lens that often distorts information or omits important details.
There was a great deal of collegial congratulations and pride taken in the quality of the collaborative research, leading to the publication of the study in the prestigious medical journal
The Lancet
.
Traboulsee’s introduction to the study was a review of the history of CCSVI from Zamboni’s work on a possible cause of or even a treatment for MS. It was a brief overview and only spoke of the initial work done several years ago and no review of more recent work being done in the US and Europe. (For a comprehensive and well-written collection of information that supports the value of venoplasty,
check out the blog written by Joan Beal
.)
There was a subtle dig at private MRI centres, including False Creek and AIM, under the term ‘commercialization’ which I suppose was meant to be critical of private centers being able to provide information unavailable in the public health care system. There was one unnamed centre that was praised for not “jumping on the bandwagon” as they opted not to provide an assessment service. Readers of my blog know that
I wish I had gone private sooner as I would have been spared a lot of abuse
. Waiting in pain for years for help was a serious failing of the beloved health care system. (One of my MS mentors believes it was because I am a woman. Unfortunately, I agree with her.)
There was a description of ‘medical tourism’ and an estimate of 3-5,000 Canadians leaving the country to have the venoplasty procedure done. The ‘perception’ of benefit was about a 50/50 split. He did say that “people have died” from complications but did say “not very many.” I have heard of perhaps three but I do know that one of the MS drugs called Tysabri has caused many more deaths (52 by 2012) and this doesn’t include drugs in clinical trials. To be honest, many of us with MS don’t always think of death as the worst possible outcome, so the value of that metric is debatable.
Traboulsee talked about the social passion of the advocates of the procedure and the information and misinformation that took place in the media.
The premise of the study was to test the hypothesis of CCSVI and if it exists. And if it does exist, is it related to MS? This is Phase I of the multi-year research and was conducted at two sites, UBC and University of Saskatchewan.
The radiologist, Lindsay Machan, spoke next. They did ultrasound and the technicians were trained by Zamboni. They also looked at blood flow using 4D Tract Imaging. (This had not been reported at all in the media and I regret having said that they didn’t measure flow in my op-ed piece.) Unfortunately, there was no real discussion or analysis of flow measures, so it is hard for me to compare with the results that I got with my scan. Dr. Raj Attariwala from AIM Medical Imaging has a degree in Biomedical Engineering and he did tell me that most doctors don’t understand or learn about fluid mechanics. I will follow up on this by getting a copy of the full article in
The Lancet
to assess this shortcoming of the presentation.
Machan talked about how tricky it was to view the veins as a Valsalva maneuver can block the blood flow and look like stenosis of the vein. They observed immobile valve leaflets in people with MS as well as healthy subjects.
Machan speculated that positive reports of venoplasty could be a placebo effect. I guess when you’re a radiologist who doesn’t see patients, it’s easy to believe that the ‘anecdotal evidence’ is questionable. He ended his portion with his belief that this research of blinding and double-blinding everyone involved will produce the best study in this area. It took the research team one year to develop the standardized protocol.
Dr. Traboulsee concluded the talk by summarizing the findings. There were 177 participants, 79 with MS and 98 unaffected. UBC and U of Saskatchewan found complete vein blockages in 1.5% using catheter venography images. (He compared this with 100% blockages in Zamboni’s original study but did not mention if the method for assessment was different, e.g., ultrasound.)
They then decided to re-look at the data and suggest that vein narrowing of 50% or more might give another view. They found that 74% of people with MS had greater than 50% narrowing, the unaffected siblings were 66% and the unrelated/unaffected were 70%. This was not what they were expecting to see, so they considered that it might be abnormal flow. Again, the abnormal flow for MS 51%, unaffected siblings 54% and unaffected 54%. It wasn’t clear to me exactly what they meant by abnormal flow and how they measured it.
So, what did this tell the researchers? They concluded that MR venography was not as good as their technique of catheter venography, and that CCSVI as described by Zamboni does not exist as narrowing of veins is common.
Does venoplasty affect the course of MS? Traboulsee acknowledged that it can’t be determined with this study alone and it’s why they will be moving forward with Phase II Treatment Trial. They have completed 7 procedures to date and will be following them very closely, including patient response outcomes.
I congratulate Traboulsee for saying that it would be disrespectful to ignore what many people are saying about changes and improvements. The research takes time.
Each of us with MS will make our own decisions about whether or not we can wait.