On May 30, 2011, I was preparing to go see a client downtown. I was eating lentil soup for lunch, when I had a huge neurological pain break through my face. I called to cancel.
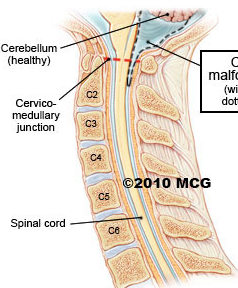
A couple of days later, we headed off on a road trip to Calgary for our goddaughter’s graduation. While on the road, I started having nerve sensations around my temple in the shower. I knew that was the first branch of the trigeminal nerve. That meant I had pain on all three branches. I was freaking out as this one was new.
I had renewed problems on my lip and roof of my mouth. I didn’t have another full breakthrough until June 9. After that, I started to have them every day, either brushing my teeth or eating. The pain would throb through my face for 15 to 30 minutes at a time. I went to see my GP on June 13 for a new neurology referral. It was easy to get in to see her that day because the rest of the city was watching the Canucks in the playoffs.
She told me that it would be difficult to get in to see the neurologist I had requested as he had a year long waiting list. I wanted somebody who was an ‘expert’ in trigeminal neuralgia and he had been highly recommended to me. My GP told me to ask to be on the cancellation list if I could let them know that I could be there on short notice.
I waited. I had trouble eating and sleeping. I kept on working the best I could. I developed a stiff neck and a fever in mid-July. By the time the Folk Festival came around, I was out of pain but had numbness on my upper lip. By July 25, I was enjoying food again. And then I received a phone call asking if I could attend an appointment with the neurologist on July 28, as there had been a cancellation. I was doing well but was pleased that I would get a chance to have an expert opinion and perhaps some attempt at a differential diagnosis.
I arrived at his office early and waited. Then I heard somebody call “Jessica?” and again, “Jessica?” Damn, I thought, he doesn’t even have my name right. A minute later I heard, “Jennifer?” and went to meet him. I shook his hand and then he introduced me to a resident. “Dr ___ is here to learn about headaches.” I replied, “I don’t have headaches. I have trigeminal neuralgia.” At this point I was wondering what I had done asking for this neurologist. I told myself to be patient. It is a teaching hospital. I used to train students too. Eventually, this doctor will get the information he needs. I had come prepared with a written history to assist as well as the report written by the oral medicine specialist I had seen in May, 2010.
I spent 1.5 hours with the resident as he examined me and took my history. The neurologist joined us for the final 30 minutes of my two hour appointment. The resident provided a summary of my history. I had to interrupt several times to correct some details.
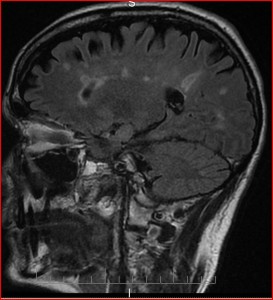
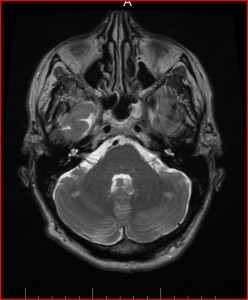
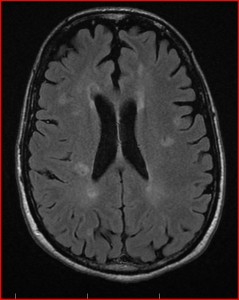
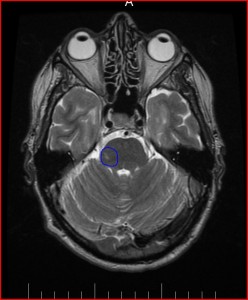
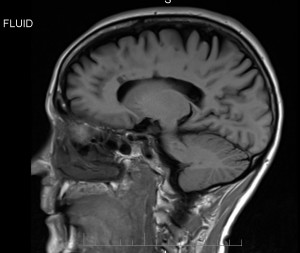
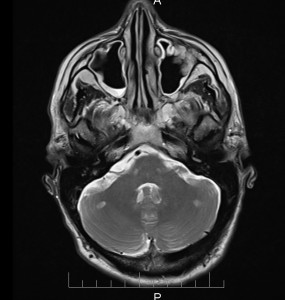
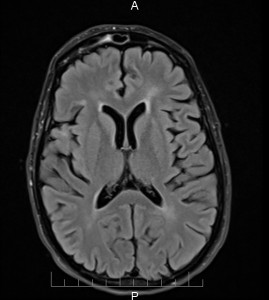
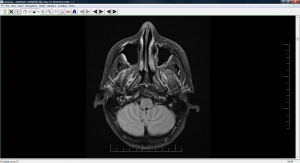
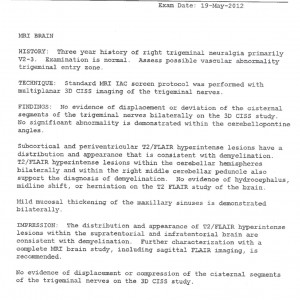
The neurologist told me that he would put in a request for an MRI on a non-urgent basis as I was managing and my symptoms did not strike him as typical trigeminal neuralgia and he doubted if the MRI would show anything. He did assure me that he could move the exam forward if necessary. And he also said that if surgery was indicated, he could make that happen quickly too. We booked a follow-up appointment for three months later.
The system here in BC seems to be that your GP gets the specialist reports and you don’t get them unless you request them. After the trauma of our interrupted trip to France, the struggle to get help with my GI problems and finding a new GP, I showed up for my appointment on October 26. While I was in the waiting room, I asked his office assistant if I could get a copy of the consult from July. I was sorely disappointed.
There were several parts of the history missing, including the introduction of the upper branch of the trigeminal nerve. There was no mention of the long bouts of pain in May and June. All that he seemed to use for his history was the report written by the oral medicine specialist who saw me once. Was I offended? Yes — it was obvious that the time I took to prepare a history was a complete waste of my time. There was no mention of the resident who examined me. So, if you read the report, you would have no idea that the neurologist didn’t examine me himself.
When I went into his office, I attempted to help him make corrections to the report. He listened a bit and made some changes but not a lot. When I read the note from the October meeting, he said “she presented me with a number of corrections to my March 2011 consultation report.” Funny, I hadn’t even been referred to him in March.
Now, I know we’re all human and we make mistakes. But these are medical records and they are supposed to be accurate. I laboured so hard to ensure the accuracy of my reports when I worked in healthcare and they carry no weight at all as I was just a “speech therapist.” Regardless, it was my professional responsibility to do my best. I would
never
have neglected to report on the fact that a student/intern/resident did the evaluation. It’s unethical. And as he sees so many patients, I am sure he by now doesn’t even remember that he didn’t do the evaluation. But I remember.
So, again, I was vulnerable. I needed to stay on good terms with this neurologist if I needed help. It’s a small city and a small medical community. He did give me some botox in my face the next month that helped a fair bit and I was grateful for that. I was losing weight as I was having so much pain and trouble eating as well as having gastrointestinal problems. He did make a couple of comments about the fact that I would benefit from taking the Lyrica pills as they would put a few pounds on me. He made lots of off-the-cuff comments like that and I found them so offensive.
Right now, knowing that I likely have MS, I can’t believe he didn’t start to look at things more seriously. He said he’d call my GP and my GI doc but I don’t think he ever did. Once I was out of his office, I was out of mind. My friend who is a pediatrician thought it could be MS. I assumed that a neurologist would at least consider it. I had spoken with the oral medicine doctor (now retired) about MS too in May 2010. He assured me that I would be in excellent hands at VGH. I’m still puzzled.