A trip to Québec

Daniel and I got back three days ago from a week-long trip to visit his family in Québec. This photo is a character named Monsieur Rigolo that his dad made from wood scraps who greets visitors at their place on the banks of the Chaudière river.
It was important for me to go because it may be my last trip to see them. The last time I was there in July 2010, I was in so much pain that I couldn’t eat. I was eating a bowl of soup with a bit curry in it when I had 3 consecutive very strong and painful shocks in my mouth. From then on, brushing my teeth or eating anything mildly spicy or acidic caused me pain.
[I called my dentist when that happened and she told me not to see any other dentist until I got home as she was afraid I’d get unnecessary work done. I remember telling her that I would be OK if somebody could put a cap on the tooth #14 in my upper right. I then referred to that tooth as ‘curry tooth’. When I got home, my dentist observed that the tooth was loose and she replaced the amalgam filling with a composite. She adjusted my bite as the previous dentist had messed up a crown. Things were pretty good after that until we discovered some gum disease in the lower right.]
I blended most of my meals after that and drank with a straw. I am the only person who has spent time with the family and gone home weighing less than on arrival. My mother in law is a great cook.
It was important for Daniel that I be there as there were two family events. His older brother celebrated his twenty-fifth wedding anniversary. And his father’s side of the family held a large reunion at Île d’Orléans, a picturesque island southeast of Québec City. The next day we explored the island with my brother-in-law and sister-in-law.

A couple of days later, we also spent an afternoon in Quebec City, then had dinner with old university friends of Daniel’s at beautiful Lac-Beauport.
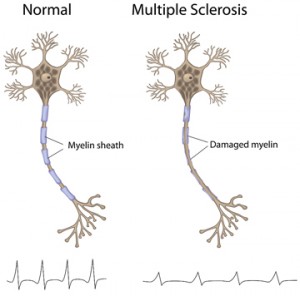
I seemed to be in the midst of a mild relapse while there. I was a bit slow on my feet and my hands were very numb at night. I was also constipated.
I’m doing better this morning. I’ve continued with the Tecfidera and I’m tolerating it quite well. I understand that it takes 3-6 months for the full effects to be realized.
Travelling is hard now and I used to really love it. Now, I have to watch what I eat, I can’t drink wine, so there is much less pleasure. I have a lot less energy.