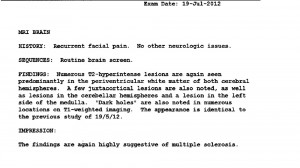
This post has taken me a while to get to, mainly because the whole ordeal was so traumatic, and it’s a long story. It gives me new insight and empathy for people who are mentally ill and who have health problems, especially if they’re subtle or invisible, like mine were. As the local neurosurgeon stated in his report, I’m a meticulous historian. I keep notes in my appointment books and I have for many years. And I keep them. I worked with enough people with brain injuries who had medico-legal cases, and I understand the importance of accurate records. I knew how problematic inaccurate records could be, and I knew that errors are more common than most people appreciate.
Before going to emergency,
I had a terrible time trying to find help
. In hindsight, I really needed to find a GP to help me. I had been trying in the summer as I was already unhappy with GP #2. She was less than helpful as I got worse, and it’s even harder to find a new doctor when you’re in distress. If my pediatrician friend had been my GP, I would have been helped at least the month before this hospitalization, and probably years earlier. He listened to me thoroughly and gave my situation a lot of thought. He suggested MS as a possibility or least as something that should be ruled out.
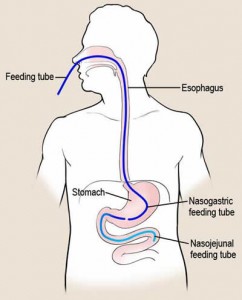
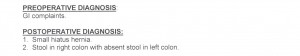
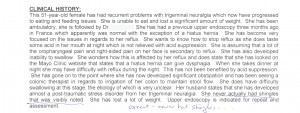
I had lost the ability to move my bowels on my own. I was hypersensitive to anything in my mouth. I slept sitting up. I ate very little. On Christmas Eve, I asked my husband to take me to the ER of the hospital where my gastroenterologist had admitting privileges, as I wanted to have his support. I was offered a meeting with a psychiatrist. I knew I wasn’t out of my mind (yet), so I walked away. We went home. Christmas Day was miserable. The next day we went back to the same hospital and refused to leave until I was admitted. We waited a long time. I asked a nurse to give me a lethal injection to put me out of my misery. They sent us home with a promise that we would be seen the next day by gastroenterology. So, on December 27, we went back and I was admitted. In the admitting ward off of the ER, the on-call gastroenterologist walked in, brusquely ordered my husband to wait outside with a word and a hand gesture, then he interviewed me.
“What are you doing here?,” he barked at me, as he stood at the foot of my bed. Wow, I thought to myself, this guy has a great bedside manner. Let’s say I was rubbed the wrong way and in my condition, I had no ability to rise above it. I have met plenty of arrogant and rude people in different situations but it was rare to encounter that attitude in a health facility. I responded, matching his attitude, “I have atypical GERD and idiopathic or atypical trigeminal neuralgia, and being a middle-aged woman, I guess that makes me ‘crazy’.” He proceeded to ask me several questions and I stuck to the facts, as well as my experiences, to the best of my ability. When he asked about my family history, I told him about my genetic family history as he was a medical doctor and that’s usually what they’re looking for. I didn’t like him at all. I figured that once I got through this and admitted that perhaps I wouldn’t see him again and then the great docs in this hospital could help me figure out what was wrong with me.
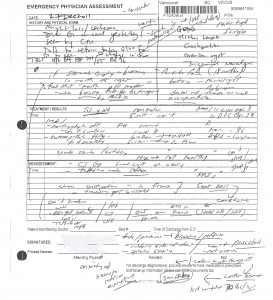
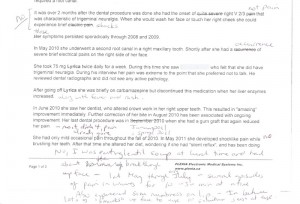
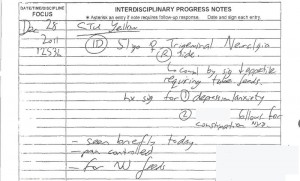
I have a copy of the notes he jotted down while speaking with me. He put some of the things I said in quotation marks. He put his own words like ‘counselor’ when I told him about my psychologist. (I would never call a psychologist a counsellor as they are two different things. A psychologist may use counselling techniques but they are so much more than ‘counsellors’.) I gave him the analogy of my mouth feeling like a pH monitor with my hypersensitivity to acidity, although by this time, I was having pain with everything I ate.
click image to enlarge
I would say these notes accurately reflected the conversation we had along with his observations, except for the emotional tone of our interaction as I didn’t like him and he was obviously annoyed by me. You can see in these notes that he initially got the information about my family correct. My mother (biological) alive at 86, my father dead of lymphoma. After he met with me, he met with my husband. Apparently, he didn’t ask my husband about my physical health or my family. All he asked my husband was, “Have there been any emotional upsets in her life recently?” and my husband told him that my mother had died the year before. That was my adoptive mother. My husband is not really familiar with how medical people work or think — that was my domain. Not once did this gastroenterologist ask for clarification from either one of us. Not a single person on the health care team ever asked about it. It would have been very easy to explain. As my psychologist put it months later, “He intercepted the football and ran all the way on his own for the touchdown.”
The unfortunate thing about these dictated electronic records is that they are available to any doctor who is treating you. So, if I get referred to another doctor, they have these at their fingertips.
[I was
treated abusively by my GP on January 18 after discharge
from the hospital. And on February 14, neurologist #3 asked me why they thought I had post-herpetic neuralgia. It’s a good thing he asked about it as that prompted me to request my records. The incorrect term came from this one specialist who went way beyond his area of specialty and jumped to several conclusions. His three reports were the only ones in my medical records that used the term post-herpetic neuralgia. When I saw my attending physician in March (as an outpatient) about the use of the term — before receiving the copies of my records — she said that it must have been a resident.]
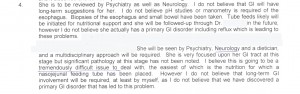
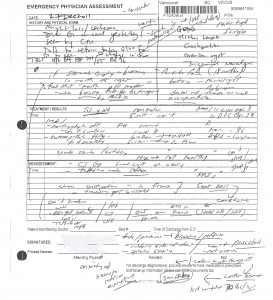
This is how the consultation report looked when it got dictated after the gastroenterologist had a chance to digest and speculate. I received these reports on Friday, April 13, 2012, four days before my sinus surgery. I was stunned. And then everything made sense.
I’ve pulled out the sections that caused me concern:

click image to enlarge
He mixed up my parents. My biological father died of lymphoma. My biological mother was alive. My adoptive father died of esophageal cancer, and my adoptive mother of lung cancer. Both my adoptive parents had metastatic cancers.
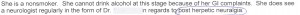
Later in his report he says this:

click image to enlarge
Obviously, I was delusional and my husband was the sane one. I didn’t know my mother was dead! At least he documented the fact that he spoke to both of us separately. Sort of a power interrogation technique, it seems.
His were the only reports that used the term post-herpetic neuralgia (nerve pain after shingles) but in this report and the two subsequent ones he did, he made reference to the fact that I had never had a rash on my face. This isn’t surprising as I have never had shingles. And he made note of it in his original handwritten note above in the upper right corner ‘never had shingles’.
click image to enlarge

click image to enlarge
As you read those descriptions, you start to realize he is expressing some doubts about the pain I was experiencing. I tried to describe how scary it was to be eating but not having bowel movements. This had been going on since mid-September. And I used an analogy to describe the sensitivity to acidity in my mouth, that he chose to rephrase in a way that made me sound really ‘crazy':
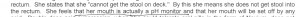
click image to enlarge
To cap it all off, he insulted my psychologist by referring to her as a ‘counsellor’ and somehow it was surprising that I’m not keen on being diagnosed by a gastroenterologist as having a conversion disorder. That was probably when I turned my back to him.
click image to enlarge
My husband joined me after his ‘interview’. I told him how unpleasant mine had been. He encouraged me to be nice as that gastroenterologist had the power to admit me or to turn us away. So, when the GI doc came back some time later, I smiled. He told us that I would be admitted. In his note he said that I was starving and would probably be back again if they didn’t admit me. We thanked him.

 Interesting that my pediatrician friend considered possible MS with the trigeminal neuralgia plus GI problems. With all those doctors and keen medical students, you might think that the question would be asked or they might say ? MS in the note. But the fact that I was seeing the top GI doc and and a well-known neurologist seems to have frozen their brains. Or they might have believed I was too old for MS, even though you can get MS at any age.
Interesting that my pediatrician friend considered possible MS with the trigeminal neuralgia plus GI problems. With all those doctors and keen medical students, you might think that the question would be asked or they might say ? MS in the note. But the fact that I was seeing the top GI doc and and a well-known neurologist seems to have frozen their brains. Or they might have believed I was too old for MS, even though you can get MS at any age.